Avoidant/restrictive food intake disorder (ARFID)
This information is about avoidant/restrictive food intake disorder (ARFID).
It looks at what ARFID is, who is most likely to develop it and why, how it’s different to other feeding and eating disorders, how it might be treated, and sources of further information and support.
About our information
We publish information to help people understand more about mental health and mental illness, and the kind of care they are entitled to.
Our information isn't a substitute for personalised medical advice from a doctor or other qualified healthcare professional. We encourage you to speak to a medical professional if you need more information or support. Please read our disclaimer.
ARFID is a mental health condition. People with ARFID don’t eat enough food, or don’t eat enough different kinds of food to meet their energy or nutritional needs. This is usually bad enough that someone with ARFID:
- loses a lot of weight
- has serious nutritional deficiencies
- needs food supplements (or even to be fed with a tube)
- has other problems with their physical health.
ARFID doesn’t happen because someone is worried about their weight and body image. It is also not caused by:
- not having access to food
- another medical condition (for example, food allergies)
- because someone is taking medication.
ARFID is different from the usual challenges that children and young people can have with trying new foods, or eating foods they don’t like. People with ARFID can be any weight, and ARFID can be diagnosed at any age.
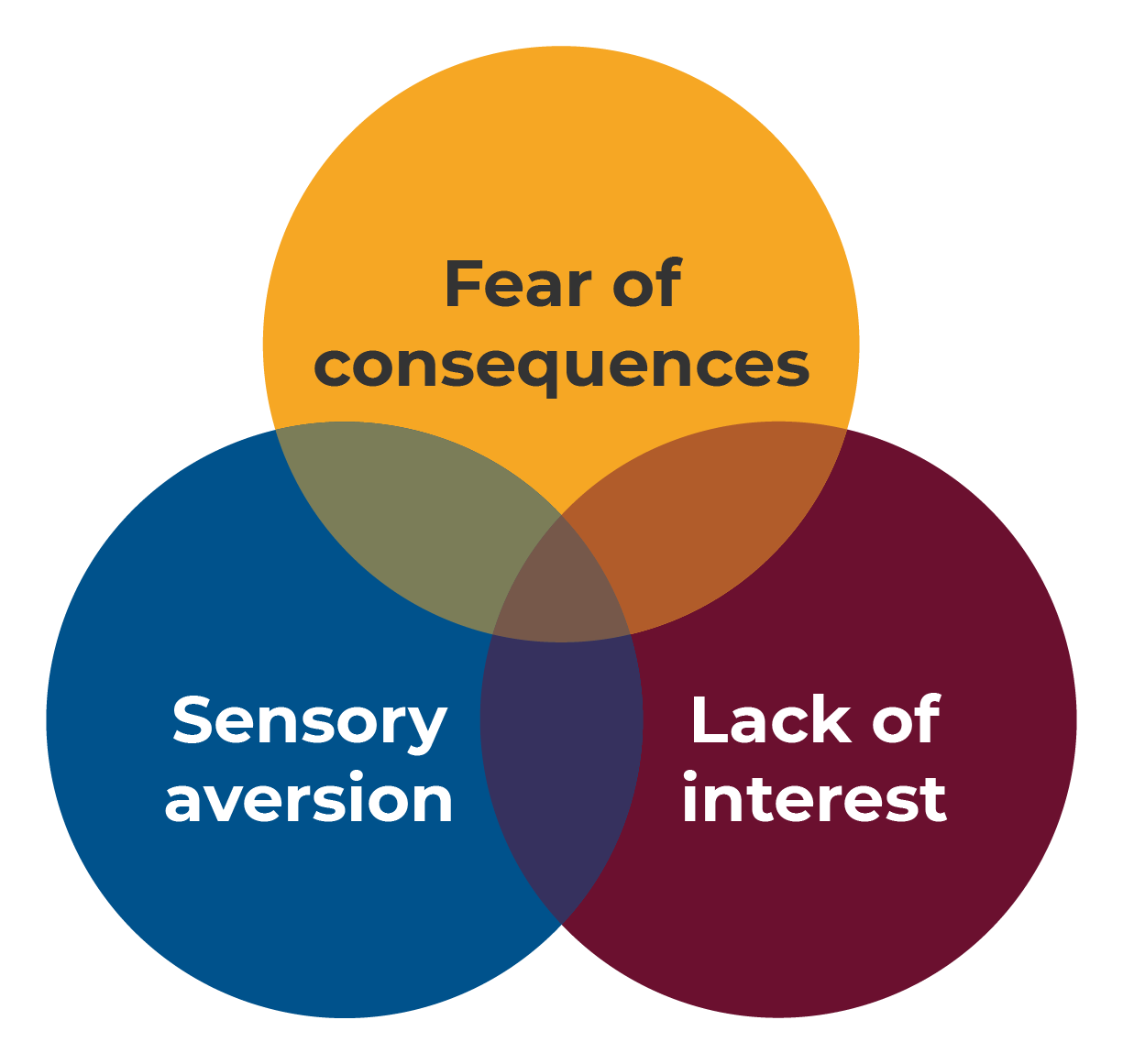 There are a few different reasons why someone with ARFID might avoid foods or eat less food. If someone is experiencing one or more of the following things, they might have ARFID.
There are a few different reasons why someone with ARFID might avoid foods or eat less food. If someone is experiencing one or more of the following things, they might have ARFID.
- Sensory aversion – Some people are very sensitive to how food tastes, feels, smells or looks. With ARFID, this will be more extreme than just disliking certain foods.
- Fear of consequences – Some people have had scary or upsetting things happen when they have eaten. E.g. choking, vomiting, stomach aches, diarrhoea or constipation. This can make them afraid or worried about certain foods, or about eating in general. They might deal with this by avoiding certain foods and only eating foods they think are ‘safe’.
- Lack of interest in food – Some people don’t feel hungry in the way that other people do, or have a ‘poor appetite’. For some people, eating can feel more like a chore than a pleasure. This can make it hard to eat enough to stay well.
One or more of these things can make someone restrict how much food or the kind of food they eat. Because of this, ARFID can look very different from person to person.
ARFID can affect lots of different things, including:
- Weight - Some people with ARFID lose weight and become malnourished. This can make them feel tired, weak and unwell.
- Nutrition - Some people with ARFID don’t eat enough to get the nutrients, minerals and vitamins they need. This can lead to conditions like anaemia, rickets and osteoporosis.
- Growth and development - Some people who have ARFID in childhood might not grow and develop in the ways that they should.
- Psychological - People with ARFID can experience a lot of anxiety and fear when they eat or think about eating certain foods.
- Social - People with ARFID might struggle in social situations that involve food and eating. This can include things like lunch times, school trips and sleepovers. It can also affect big events like birthday parties or weddings. We often get to know new people by eating with them, so ARFID can make it hard to meet new people. This can be isolating and lonely.
These affects can be particularly worrying for young people. This is because nutrition is so important for healthy physical and mental development.
People with ARFID won’t necessarily look a certain way. However, they are often underweight, or have lost a lot of weight. ARFID has often been going on for a long time before anyone realises it’s a problem.
People with anorexia and bulimia tend to think a lot about their weight and how their bodies look. This changes what and how much they eat.
However, the way people with ARFID eat doesn’t seem to be affected by how they feel about their weight or body.
You can’t have ARFID and anorexia or bulimia at the same time. If someone has symptoms of ARFID, but also:
- has worries about their weight or body
- deliberately wants to lose weight
- or tries to control their weight by making themselves sick
this is likely to be anorexia or bulimia, and not ARFID. This is important to know, as the treatment is different.
However, people with ARFID can develop anorexia or bulimia in the future.
Autistic people who have anorexia or bulimia might seem to have some of the symptoms of ARFID, such as avoiding certain foods.
No, ARFID is a diagnosable clinical condition. Unfortunately, it is sometimes misunderstood as ‘picky eating’ or bad behaviour in children and young people.
People with ARFID will struggle to eat certain foods and feel upset when they try to. They will also need more help than usual to try new foods.
ARFID can affect anyone, but is more common in:
- children and young people aged 4-14 years old, though it can happen to anyone at any age
- boys
- people with other health problems, including anxiety and ADHD
ARFID is also more common in autistic people.
One reason for this is that autistic people can have sensory differences. This means that they experience their senses and sensations in a different way to people who aren’t autistic. This can make eating some types of food especially difficult.
If an autistic person has challenges with eating, this doesn’t mean they definitely have ARFID.
In the past ARFID was known by lots of different names, so there isn’t much information available about how common it is.
In one study, children aged 8-13 were asked to fill out a questionnaire. These questionnaires showed that about 1 in 33 of these children showed signs of ARFID.
In the past, some children were diagnosed with ‘feeding disorder of infancy or early childhood’. Today, these children would be diagnosed with ARFID.
More research is needed to understand how ARFID should be treated. However, there are a number of different things that can be done to treat someone who has ARFID.
How ARFID is treated will depend on what is causing it. Normally, treatments for ARFID focus on:
- fixing any physical health problems
- working out which foods someone is avoiding and why
- and helping them to try the foods they are avoiding.
If you or someone you know is experiencing some of the symptoms of ARFID, speak to your GP.
Treating physical health problems
If someone with ARFID has developed physical health problems, these will need to be treated first.
Treatments to help with nutritional deficiencies and weight loss include:
- multivitamins
- mineral supplements, e.g. zinc or iron
- medication to increase appetite
- advice on alternative and ‘safe’ foods for the person to eat. This might help them avoid becoming nutritionally deficient
- if someone is experiencing severe anxiety, in some cases anxiety medication might be helpful for a short time
Medical professionals should make sure that someone with ARFID doesn’t have any other medical conditions that are making it hard for them to eat. For example, a health problem that makes them lose their appetite or have trouble digesting.
Psychological treatments
Once any physical health problems have been treated, psychological treatments can be started. These can help to change someone’s patterns of eating, and should be adjusted depending on how they are able to discuss and make changes to their eating.
These treatments include:
Cognitive behavioural therapy (CBT)
CBT is a type of talking therapy. It can help someone to learn more helpful ways of thinking and reacting to challenging situations.
There is a type of CBT developed specifically for people with ARFID. In this type of therapy, people set goals and make changes to the foods they eat. They will work with a therapist to expose themselves to new foods or foods they are avoiding.
Graded exposure
This is a CBT technique that can be used to help someone with ARFID change the way they act around food.
In graded exposure for ARFID, foods are ranked by how much anxiety they cause. The person will work with their therapist to make a plan to try these foods. They will work towards realistic goals, and be given the tools to help manage their anxiety along the way.
This can be helpful for people with ARFID who are scared of eating because of negative experiences they have had in the past. E.g. vomiting or choking.
Other behavioural approaches
Here are some approaches that can be helpful for people who have sensory problems:
- Food chaining – This involves finding a food that someone is able to eat and slowly introducing them to very similar foods. These foods will have similar sensory qualities. For example, if someone only eats chips, they might be introduced to a different kind of chip, then roast potatoes, and so on.
- The Sequential Oral Sensory (SOS) approach – The SOS approach is aimed at children and young people. In this approach, a therapist helps someone to try new foods. The methods they use will depend on the age or developmental stage of the person.
Family-based approaches
Parents and carers can be the main source of support for someone with ARFID, and family-based approaches take this into account. Strategies used in family-based approaches include:
- teaching the family skills that allow them to help the person with ARFID
- helping with structure and routine at mealtimes
- making changes to the home environment
- teaching ways to deal with anxiety.
There is a specific family-based approach that has been developed for ARFID.
Autistic people experience and interact with the world differently. Because of this, changes might need to be made to their treatment. These changes are called accommodations.
The kinds of accommodations that might be helpful for autistic people with ARFID include:
- Providing a peaceful environment to eat in. This should be away from noise, chaos, interruptions, and other people who are eating.
- Allowing flexibility around mealtimes. This could mean snacking throughout the day, or eating foods in a non-typical way. E.g. eating breakfast foods at dinner time.
- Helping the person to explore how food smells or feels before trying to eat it, to help them to cope with change.
- Letting the person ‘stim’ whilst eating. ‘Stimming’ can include things like standing or moving, and using fidget toys or screens.
- Aiming for consistency and avoiding unpredictable changes. For example, allowing someone to eat in front of the TV one day, then making them eat at the dinner table on another, should be avoided.
- Understanding that the person might struggle to know when they are hungry or full.
- Avoiding hiding foods inside of other foods to encourage the person to eat things they don’t want to. Autistic people often notice small changes, and this might cause them to lose trust in you.
Beat, ARFID – Information on ARFID from the UK’s eating disorder charity.
National Centre for Eating Disorders, ARFID – Information on ARFID from an organisation that offers information to people living with eating disorders and professionals working with people with eating disorders
ARFID Awareness UK – A charity dedicated to raising awareness and furthering information about ARFID.
Cognitive-Behavioral Therapy for Avoidant/Restrictive Food Intake Disorder: Children, Adolescents, and Adults, Jennifer J Thomas – This book is written by experts in ARFID, and looks at CBT and how it can be used to treat ARFID.
This information was produced by the Royal College of Psychiatrists’ Public Engagement Editorial Board (PEEB). It reflects the best available evidence at the time of writing.
Authors: Dr David Ochando and Dr Dasha Nicholls
Expert reviewers:
- Dr Agnes Ayton, Chair of the Faculty of Eating Disorders Psychiatry
- Dr Peter Carpenter, Chair of the Neurodevelopmental Psychiatry Special Interest Group (SIG)
- Dr Conor Davidson, RCPsych Autism Champion
- Autistic Doctors International
Special thanks to the people with lived experience of ARFID who shared their thoughts on this resource.
Published: Dec 2022
© Royal College of Psychiatrists










