Stopping antidepressants
This information is for anyone who wants to know more about stopping antidepressants.It describes:
- why someone might choose to stop taking their antidepressant
- how to do so safely
- symptoms that you may get when stopping an antidepressant
- some ways to reduce or avoid these symptoms.
This patient information accurately reflects recommendations in the NICE guidance on depression in adults.
About our information
We publish information to help people understand more about mental health and mental illness, and the kind of care they are entitled to.
Our information isn't a substitute for personalised medical advice from a doctor or other qualified healthcare professional. We encourage you to speak to a medical professional if you need more information or support. Please read our disclaimer.
Antidepressants are medications prescribed for conditions such as depression, generalised anxiety disorder and obsessive-compulsive disorder (OCD). You can find out more about how they work, why they are prescribed, their effects and side-effects, and alternative treatments in our separate resource on antidepressants.
Antidepressants usually need to be taken for at least 6 months after your symptoms have gone away. However, this should be reviewed by your prescriber regularly. People with severe or recurring mental illness might need to take antidepressants for longer.
There are lots of reasons that people choose to stop taking their antidepressants, including:
- the mental health problem they were having has got better
- the antidepressants aren’t working
- the antidepressants are giving them unpleasant side effects
- they don’t want to take antidepressants anymore
If you are taking antidepressants, and you experience any of these things, speak to your prescriber. They can help you to decide whether stopping antidepressants is right for you and how to do it safely.
Antidepressants should not usually be stopped suddenly. This can lead to you developing withdrawal symptoms and increase the chance of you becoming unwell again. Withdrawal symptoms are different for everyone. They can be different for individual antidepressants (see Appendix 1).
Most people can gradually stop taking their antidepressants over a few weeks or months, by taking smaller doses and then stopping completely. This is called ‘tapering’. This can reduce the risk of you getting withdrawal symptoms, or mean that any symptoms you have are less severe.
Everyone should taper their antidepressants, but some people (usually people who haven’t been using them for very long) only need to reduce in a couple of steps.
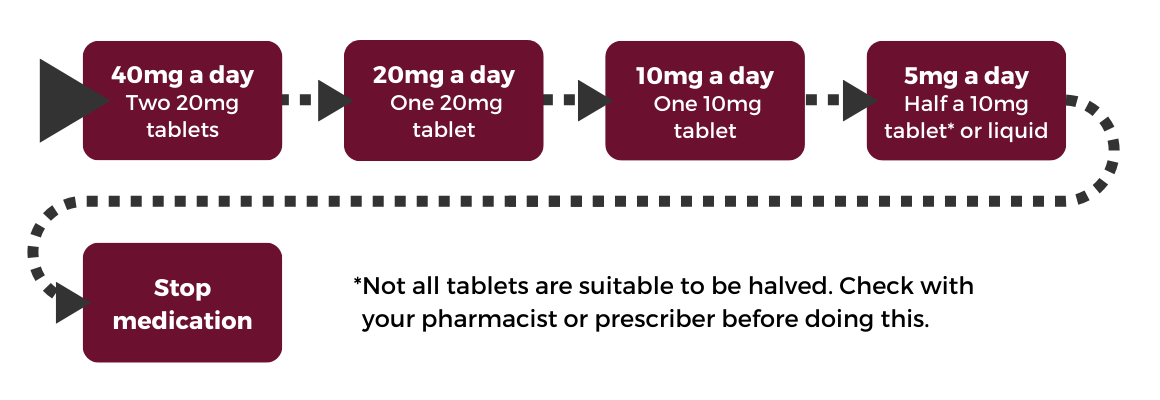
If you are stopping your antidepressants after a short time, your prescriber might recommend that you do something like the example below. Here, you would reduce your current dose by approximately 50% every 2-4 weeks, and stop entirely once you were at a low dose.
If you struggle to taper this quickly, and get withdrawal symptoms when you try to stop taking them, you will need to taper your antidepressants more slowly. It is important to reduce the dose in a way that is right for you and does not cause you problems.
This resource aims to help you avoid getting any withdrawal symptoms, or get the fewest possible. Talk this over with your prescriber so you can find the best way to stop taking them.
NICE guidelines suggest that for some, withdrawal symptoms can be mild and go away relatively quickly, without the need for any help. Other people can have more severe symptoms which last much longer (sometimes months or more than a year).
At the moment we cannot predict who will get the more serious withdrawal symptoms.
Symptoms of antidepressant withdrawal
If you do get any of the symptoms listed below, tell your prescriber.
You may notice:
- anxiety which comes and goes, sometimes in intense 'surges'
- difficulty in getting to sleep and vivid or frightening dreams
- low mood, feeling unable to be interested in or enjoy things
- a sense of being physically unwell
- rapidly changing moods
- anger, sleeplessness, tiredness, loss of co-ordination and headache
- the feeling of an electric shock in your arms, legs, or head. These are sometimes called ‘zaps’ and turning your head to the side can make them worse.
- a feeling that things are not real (‘derealisation’), or a feeling that you have ‘cotton wool in your head’
- difficulty in concentrating
- suicidal thoughts
- queasiness
- dizziness (this is usually mild, but can be so bad that you can’t stand up without help)
- a feeling of inner restlessness and inability to stay still (akathisia).
See Appendix 2 for a list of other reported symptoms.
This is still poorly understood. Brain chemicals called neurotransmitters (such as serotonin and noradrenaline) are involved. They allow nerve cells to communicate with each other by acting on nerve endings. Antidepressants are thought to increase levels of these chemicals in the space between nerve cells in the brain, and in the nerves throughout the body and gut. Over time, the brain and body seem to slowly adjust to these increased levels.
If an antidepressant is stopped too quickly, the brain and body will need time to adjust back again. The sudden lowering of neurotransmitter levels seems to produce withdrawal symptoms, while the brain adjusts to the change. The more gradual the changes, the milder and more tolerable symptoms should be. Or they may not happen at all.
This is why it is usually best to stop an antidepressant slowly.
Between a third and half of people who take an antidepressant will experience such symptoms to some extent. We cannot yet predict who will get these symptoms.
The risk seems to be greater if you have taken a high dose for a long time. But it can happen if you have taken an antidepressant for just a short time too. It can also depend on the type of antidepressant you have been taking. You are more likely to get these symptoms (and for them to be worse) if you stop taking an antidepressant suddenly or if you reduce the dose quickly.
Some withdrawal symptoms can feel like the symptoms you had before you started the antidepressant. The low mood and difficulty in sleeping can feel like the symptoms of depression. Panicky feelings are a common symptom of withdrawal and can also happen in anxiety. In this case, you should talk to your prescriber. You may need to increase your dose temporarily and then reduce your dose more gradually to reduce your withdrawal symptoms.
If you do get withdrawal symptoms, you can still stop your antidepressant, but you may need to do so more slowly. See the section on ‘When and how to stop antidepressants’.
These are some of the ways you and your prescriber can tell whether you are having withdrawal symptoms or whether it is the symptoms of a return of anxiety or depression:
When the symptoms start
Withdrawal symptoms normally start soon after your medication is reduced or stopped. This may be one or two days for some antidepressants – or even after missing a single dose. Usually they take a few days to start, and then get worse.
The return of depression or anxiety usually takes longer – typically weeks or months. Some antidepressants, like fluoxetine, take a lot longer to leave the body. So, with these, symptoms can start days or even weeks after stopping or reducing your dose. This can make it harder to tell if symptoms are due to withdrawal or the return of your original symptoms of anxiety or depression.
There have been reports of other antidepressants causing withdrawal symptoms that start weeks after stopping. The reasons for this are not well understood.
The kind of symptom
Some withdrawal symptoms are not things you will have experienced when you had anxiety or depression. For example, ‘electric shocks’ or ‘zaps’ or more subtle feelings you have not experienced before. People often say, “I’ve never felt this before” or “This doesn’t feel like my depression.”
How quickly they go away if you restart the antidepressants
Withdrawal symptoms usually improve quickly (in days or even hours) if you restart your antidepressant. This is much quicker than the weeks that antidepressants will normally take to relieve symptoms of anxiety or depression that have returned.
Stopping an antidepressant can give you unpleasant withdrawal symptoms, which stop if you start taking it again.
It may feel as though you are addicted to the antidepressant if you can’t stop taking them when you would like to. This is not quite the same as being ‘addicted’.
Addiction generally means that you:
- feel an urge or craving to use a substance
- lose control over your use of the substance
- experience pleasure, or ‘a high’ when you use it
Addiction can happen with substances such as alcohol, nicotine and benzodiazepines.
With antidepressants, it can be hard to stop taking them, but this is more accurately described as physical dependence.
The term ‘physical dependence’ has become confused with addiction. Physical dependence means that your body has adapted to the presence of a substance or medication.
This produces tolerance and withdrawal effects because the body ‘misses’ it when it is gone. A drug does not need to produce a ‘high’ to be dependence-forming.
How long you take an antidepressant for depends on why you were prescribed them and whether you have had to take them before. Ask your prescriber when is best to start to reduce and then stop taking your antidepressant.
You may need to balance:
- the benefits that you get from an antidepressant, such as relief from your symptoms of anxiety or depression
with:
- the problems that can occur after using them for a long time. These may include increased side-effects such as weight gain. Some people find their antidepressants seem to stop working for them as time goes on.
When you agree that it is time to stop, your prescriber can help you put together a tapering plan. How slow this plan should be is different for everyone.
If you have been taking an antidepressant for only a few weeks you may be able to reduce, and stop, over a month or so. Even if you have only mild (or no) withdrawal symptoms, it is best to do this over at least four weeks.
If you have been taking antidepressants for many months or years, it’s best to taper more slowly (again, at a rate you find comfortable). This will usually be over a period of months or longer. It’s also best to reduce the dose slowly if you have had withdrawal symptoms in the past. Dose reductions will usually get smaller as the dose decreases. Some people need to get down to a very low dose before stopping, as low as 2% of the original dose.
Remember, if you do get withdrawal symptoms it doesn’t mean that you can’t stop your antidepressant. You will just need to:
- taper more slowly
- with smaller reductions in dose
- over a longer period of time.
Only occasionally, where an antidepressant causes serious side-effects, should it be stopped suddenly, without tapering. If this does happen, see your prescriber immediately.
There is some general advice on how to do this below. However, it is best to work this out with your prescriber, so that they can prescribe the appropriate preparation and dose(s) for you. They will be able to work out any special requirements with your pharmacist, so that the prescription is tailored to what you need.
Don’t try missing medication on some days. In most cases, this will lead to the amount of the drug in your body fluctuating and make withdrawal symptoms more likely. Fluoxetine stays in your body longer than other antidepressants and could be taken on alternate days. You should speak to your prescriber about whether you should do this or not.
You may be able to start, as a test, reducing your regular dose by a quarter (25%) or a half (50%). Allow two to four weeks to adjust to the new dose, to see how things go.
If you don’t get any distressing symptoms, try a further reduction of a quarter (25%) or a half (50%) of the current dose. Allow another 2 to 4 weeks and repeat, with further periods of lowering the dose and waiting if needed.
If uncomfortable symptoms develop with your first dose reduction, or at any further reduction, stop the reduction. Go back to the last dose at which you felt comfortable and wait until you feel ready to try again. This might mean you need to use a more gradual taper, reducing by smaller amounts like 10% or even 5%.
If you have been taking antidepressants for longer
If you have:
- been taking antidepressants for many months or longer
- developed distressing withdrawal symptoms when you previously tried to reduce or stop your antidepressants
- are taking an antidepressant with a high risk of withdrawal symptoms
it is probably best, right from the start, to use more gradual reductions. For example, a twentieth (5%) or a tenth (10%) of the original dose. Speak to your prescriber regularly, so that they can keep an eye on how it is going.
Long-acting antidepressants, like fluoxetine, can take weeks to leave your body (most take just days). So, any withdrawal symptoms may develop several days, or even weeks, after reducing the dose. It is best to wait at least four weeks to see if withdrawal symptoms start before making the next reduction.
No matter how low the dose you get to, you can still get withdrawal symptoms when you stop completely. If this happens you may need to re-start the medication at a low dose for a while before starting to taper again.
If you start to get suicidal thoughts or ideas when reducing and stopping an antidepressant, this could be a withdrawal symptom, or the return of depression. Speak to your prescriber immediately. They will probably suggest that you go back to the last dose at which you felt well. Make sure you know how to get help quickly if you need it.
A note on availability
How you reduce your dose of antidepressant will depend on what dosages are available in tablet and liquid form in the UK. If the antidepressant you are on isn’t available in a liquid form, you may need to change to a similar antidepressant that is available as a liquid. Or you may need to use the other options outlined below. Your prescriber or pharmacist can advise you on how best to do this.
Tapering strips are one possible option. These are a roll or strip of pouches containing consecutively slightly lower doses to be taken each day. They are not licensed by the Medicines and Healthcare products Regulatory Agency (MHRA) in the UK. This means that your prescriber might decide to use a licensed medicine instead.
The General Medical Council (GMC) says that medical professionals should aim to use licensed medications but can use unlicensed medications if there is no licensed alternative.
Regular monitoring will allow you and your prescriber to recognise any problems quickly, particularly if you have to switch from one antidepressant to another.
Before you start tapering your medication, you should agree your tapering plan with your prescriber. They will be able to advise you on how to do so safely.
Below you will find example plans for tapering at different speeds. In your plan, you may not want or need to follow every step. But some people will find that they need to.
The time between dose reductions should be as long as it takes for any withdrawal symptoms to disappear or improve.
Some people are able to stop taking their antidepressants using only tablets. If you are experiencing withdrawal symptoms and are struggling to come off your antidepressants, you may need to use both tablet and liquid antidepressants to take smaller doses.
Using liquid needs to be very carefully managed so that there are no mistakes with the dose. Speak to your prescriber or pharmacist if you are moving from tablet to liquid, to make sure that you are converting your dose correctly.
Be aware also that the same liquid medication can come in more than one strength. For example, there may be a 5mg/5ml and a 1mg/5ml formulation available. It is important to carefully check the dose you are taking, and not rely on the amount of liquid.
How are the numbers in these examples calculated?
Example 1 uses proportional tapering. This means that each step is calculated as a percentage of your most recent dose, not your original dose. For example:
- If you are taking 20mg of a medication and want to reduce this by 25%, you need to work out 25% of 20mg, which is 5mg
- In reducing your dose by 5mg you will go down to taking 15mg
- If you want to then go down by another 25%, you would work out 25% of 15mg. This is 3.75mg
- You would reduce your current dose of 15mg by 3.75mg. This would take you down to 11.25mg
Reducing in a proportional way will mean you need to make smaller and smaller reductions as you get to lower doses.
Example 2 uses hyperbolic tapering. This is based on an understanding of how antidepressants affect the brain. Small doses of antidepressants have much larger effects on the brain than we might expect, so tapering needs to be slower at lower doses.
Hyperbolic tapering involves very similar reductions to the simple proportional tapering explained above. However, there are some differences. Some of the doses suggested in Example 2 do not exactly follow the proportional rule.
Example 1
In this example, you would reduce your current dose by approximately 50% every 2-4 weeks.
Some people may need to reduce more slowly still, which you can see in Example 2.
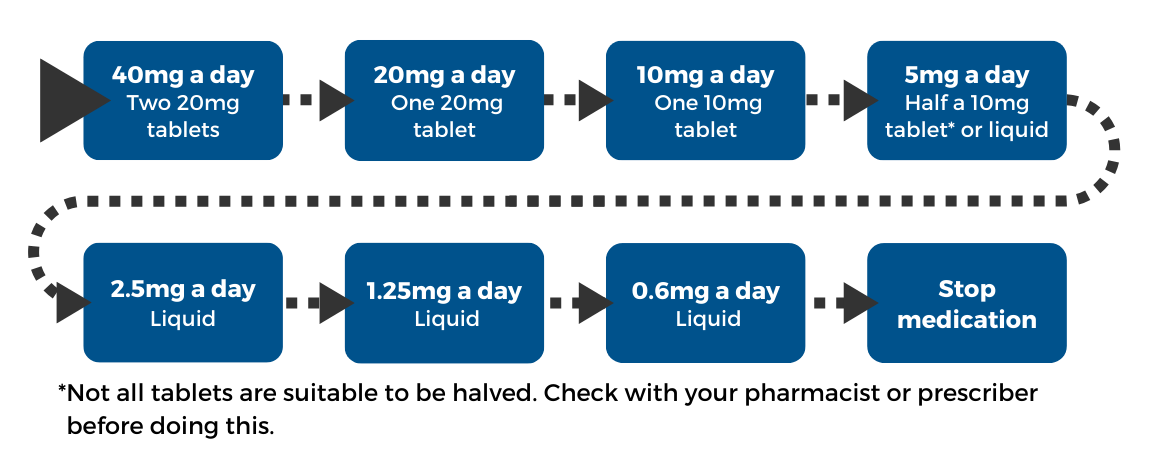
Example 2
In this example, you would reduce your dose by approximately 10% every 2-4 weeks. All steps are not exactly 10% dose reductions because this example is based on hyperbolic tapering (see above). Some people may need to reduce more slowly. For example, reducing by approximately 5% every 2-4 weeks.
To get the small doses below, you will need to use a combination of tablet and liquid antidepressants, or just liquid antidepressants. This is because tablet antidepressants do not come in amounts small enough to reduce your dose this slowly.
We will explain the principles of how this is done further on in this resource. You should speak with your prescriber to find out the best way for you to get the dose you need to taper safely.
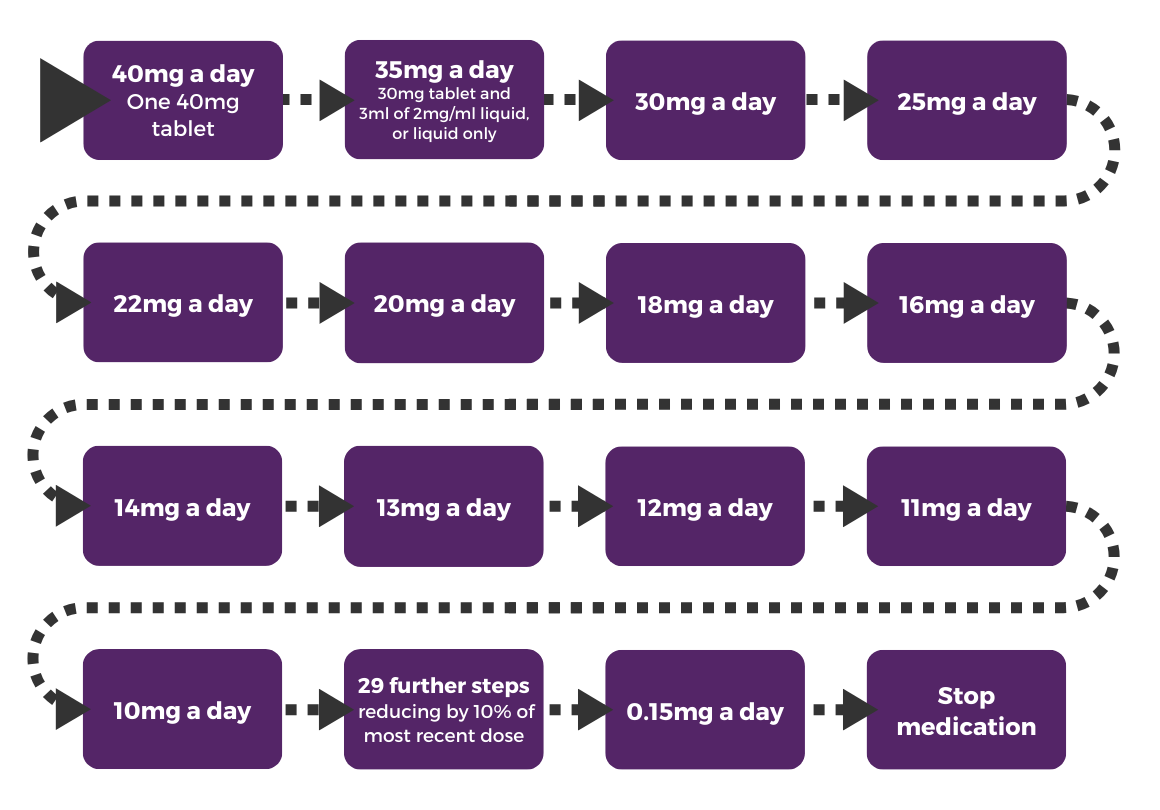
See Appendix 3 for the complete 38-step plan.
The tapering plan that is best for you will depend on lots of things, such as:
- the medication you are taking
- how long you have been taking the medication
- the dose you are taking to start with
- how strong your withdrawal symptoms are or have been in the past.
The most important thing is that these tapering plans are just starting points and should be adapted to your experience of tapering.
If you have no trouble tapering
If you have no trouble at all making reductions, then you may be able to speed up your tapering plan. You might be able to leave less time between dose reductions or take less steps. This can help ensure you are not taking your medication for longer than necessary.
If you experience withdrawal symptoms
If your withdrawal symptoms are too severe then your tapering plan should be stopped or slowed down. This might mean:
- making smaller dose reductions
- leaving more time before making a dose reduction
- both of the above
We have suggested some commonly used antidepressants that might be appropriate for the two styles of tapering. More examples are included in the appendices at the end of this resource.
Example 1 might be a suitable starting point for people taking the antidepressants in the ‘moderate, low or lowest risk’ columns in Appendix 1 at the end of this resource.
- Citalopram
- Escitalopram
- Fluvoxamine
- Sertraline
- Trazodone
- Fluoxetine
- Amitriptyline
Example 2 might be suitable starting point for people taking the antidepressants in the ‘highest risk’ column in Appendix 1.
- Duloxetine
- Mirtazapine
- Paroxetine
- Venlafaxine
This is because the higher the risk of withdrawal symptoms, the slower you will need to taper.
However, the example you follow will depend on your individual needs. You should adjust your tapering plan as you go, depending on the withdrawal symptoms you experience, rather than choosing a plan and sticking to it no matter what.
Some people will need to taper down to smaller doses of their antidepressants than is available in tablet form. This is to avoid developing withdrawal symptoms. To do this, you might be able to use a liquid antidepressant and dilute it.
Below is an example that can help you to understand the principles of diluting liquid antidepressants to taper off your medication. It is best to discuss this with your prescriber or pharmacist so you feel confident to undertake a process like the one below.
Example
In this example, you have a liquid antidepressant.
The liquid comes with a dropper mechanism that dispenses a drop of liquid. This drop is approximately 0.05ml and contains 2mg of the drug.
To taper off this medication, you need to take a dose that is less than 2mg, but the dropper mechanism will not allow you to do this.
To measure smaller doses, you will need to remove the dropper mechanism from the bottle and use an oral syringe.
You may also need to dilute the liquid in water to create a weaker solution. This is because the smallest amount of solution that can be accurately measured with an oral syringe is about 0.2ml.
You can use oral syringes to measure out exact amounts of liquid antidepressant and water. These syringes come in 1ml, 5ml and 10ml versions.
You can buy these oral syringes from a pharmacy or online or ask your prescriber to prescribe them if you receive your prescriptions for free.
Example instructions
In this example, you are using a 40mg/ml liquid antidepressant. This means that every 1ml of this liquid antidepressant contains 40mg of the drug.
Therefore, every 0.5ml of this liquid antidepressant contains 20mg of the drug.
You are aiming to take just 1mg of the drug. To do this, you need:
- A 1ml oral syringe
- A container with a cap that won’t leak when you shake it
- Your liquid antidepressant
Steps
- Measure out 0.5ml of the liquid antidepressant with a 1ml oral syringe
- Put this into the container
- Measure out 9.5ml of water with your 10ml oral syringe
- Add this to the container with the liquid antidepressant
- Mix vigorously by shaking
- This will give you 10ml of diluted solution, which will contain 20mg of the drug
- Clean your 1ml oral syringe with water
- Use your clean syringe to take 0.5ml of this diluted solution, which will contain 1mg of the drug
- Dispose of the rest of the diluted solution*
You can make up other doses with the same approach. However, you will need to know:
- How much of the drug is contained in the liquid antidepressant you are using (this is different for different antidepressants)
- The equivalent dose in a tablet which may not always be the same (for example 8mg citalopram in liquid form is equivalent to 10mg of citalopram in tablet form)
This should make it possible for you to create smaller doses of your antidepressant, allowing you to follow a slower tapering plan.
Always speak to your prescriber before starting a tapering plan.
*The manufacturer leaflet (also called the ‘Summary of Product Characteristics’) says once mixed with water, the solution should be consumed ‘immediately’. This means that after taking your dose of diluted solution, you should dispose of the rest and mix a new batch when you need to take your medicine next. Ask your prescriber for the manufacturer leaflet for the medication you are using.
Using liquid versions of antidepressants has been explained above. There are also other ways to make up smaller doses of antidepressants for tapering.
This information aims to help inform people about different forms of tapering. You should not attempt any of these methods without speaking to your prescriber first.
Tablet splitting
Not all tablets are suitable to be split, even if they have a line down the middle. Check with your pharmacist or prescriber before doing this. The easiest way to split tablets is by using a tablet cutter. How you do this will depend on the shape of the tablet:
- Round tablets can usually be cut into halves and quarters, unless they are particularly small.
- Caplets or capsule-shaped tablets will sometimes have a line down the middle so that they can be broken in half. This can be done more accurately with a tablet cutter.
Tablet cutters usually have collecting trays or other ways of collecting the pieces of tablet.
Depending on how much of the tablet you are trying to take, you may want to cut your tablet into halves or quarters. It isn’t possible to cut less than a quarter accurately with tablet cutters.
Tablets that are not round can generally only be divided into halves accurately. You should not try to quarter this shape of tablet, as it might not be accurate.
Example
You have a 40mg tablet and want to take 10mg.
For some tablets you could achieve this by quartering the tablet, as long as the tablet does not fall apart as it is being divided. To do this, you would use the tablet cutter to cut the tablet in half. You would then take each of these halves and cut them in half.
You would then have four quarters, each containing approximately 10mg.
You would take one of these quarters for each of the next four doses. This means that even if the quarters are not perfectly cut, you will take the right amount in total.
Counting or weighing beads
Some medications, such a venlafaxine and duloxetine, come as capsules containing small, ‘slow release’ beads. This means that the beads have a coating that allows the drug inside them to be released into the body slowly. Check with your pharmacist that the brand you are taking does contain these beads as this is not the case for all brands.
In this case, the capsules can be carefully opened, and the beads emptied into a container. These beads can be counted or weighed to make smaller doses. The beads are thought to be stable once removed from the capsules. This means that you can keep them in an airtight bottle protected from light (e.g. an amber medicine bottle) for a few days before taking them.
Example
You have a 75mg capsule of venlafaxine. You empty the beads out and count them.
The capsule contains 200 beads. This means that 160 beads will contain 60mg of venlafaxine.
Be aware that there is some variation in the size of these beads. Weighing beads can therefore be more precise than counting. Weighing tiny amounts requires special scales and a draught-free environment.
Before swallowing these beads you should put them back into a capsule. Venlafaxine beads can be sprinkled on a spoon of yoghurt to make them easier to swallow so that they don’t irritate your throat. Duloxetine beads should not be mixed with food or liquid.
Dispersing capsule powder in water
Some capsules contain powder. As outlined by the NHS Specialist Pharmacy Service, these capsules can be opened and the contents dispersed in water.
Example
You have a 20mg capsule. You want to take 4mg of the antidepressant.
You mix the powder in the capsule with 100ml of water. This mixture now contains 1mg in every 5mls.
You use a syringe to take 20mls of the mixture, which contains 4mg.
Any mixture made should be shaken vigorously before being taken to make sure the medication is evenly distributed in the liquid. Make sure you throw away any remaining liquid after you have taken what you need.
Dispersing tablets in water
Many antidepressants in tablet form can be placed in water, and will break apart and mix in with the water. This is called disintegration. Often this will happen in a couple of minutes, but it can take a bit longer. Once disintegrated, the tablet contents will need to be dispersed in the liquid by mixing or shaking the tablet in the liquid.
The process can be sped up by crushing the tablet with the back of a spoon first.
Example
You have a 20mg tablet but want to take 2mg.
You mix the tablet with 100mls of water. This mixture will contain 1mg of drug in every 5mls of mixture.
You can then use a syringe to take 10mls of this mixture, which will give you 2mg of the drug.
This mixture should be shaken vigorously before being taken to make sure the drug is evenly distributed in the liquid. Make sure you throw away any remaining liquid after you have taken what you need.
| Highest potential risk | Medium potential risk | Low potential risk | Lowest potential risk |
|---|---|---|---|
Desvenlafaxine | Amitriptyline | Dosulepin | Agomelatine |
Duloxetine | Bupropion | Mianserin | Lofepramine |
Isocarboxazid | Citalopram | Trimipramine | |
Mirtazapine | Clomipramine | Vortioxetine | |
Moclobemide | Desipramine | ||
Paroxetine | Doxepin | ||
Phenelzine | Escitalopram | ||
Tranylcypromine | Fluoxetine | ||
Venlafaxine | Fluvoxamine | ||
Imipramine | |||
Milnacipran | |||
Nefazadone | |||
Nortriptyline | |||
Reboxetine | |||
Sertraline | |||
Trazodone | |||
Vilazodone |
| Physical symptoms | Sleep symptoms | Emotional symptoms |
|---|---|---|
| Nausea | Insomnia | Anxiety |
| Headache | Increased dreaming | Depression |
| Dizziness | Vivid dreams | Panic |
| Abdominal cramps | Nightmares | Agitation |
| Diarrhoea | Irritability | |
| Fatigue | Mood changes | |
| Flu-like symptoms | ||
| Electric shock sensations (‘zaps’) | ||
| Loss of appetite | ||
| Visual disturbances (double vision; visual trailing) | ||
| Palpitations | ||
| Missed beats | ||
| Sweating | ||
| Flushing | ||
| Tremor | ||
| Tinnitus | ||
| A feeling of inner restlessness and inability to stay still (akathisia) |
| Step | Dose (mg) | Tablets or liquid |
|---|---|---|
| 1 | 40 | Tablets |
| 2 | 35 | Half tablets* or liquid |
| 3 | 30 | Tablets |
| 4 | 25 | Half tablets* or liquid |
| 5 | 22 | Liquid |
| 6 | 20 | Tablets |
| 7 | 18 | Liquid |
| 8 | 16 | Liquid |
| 9 | 14 | Liquid |
| 10 | 13 | Liquid |
| 11 | 12 | Liquid |
| 12 | 11 | Liquid |
| 13 | 10 | Liquid or tablet |
| 14 | 9 | Liquid |
| 15 | 8.1 | Liquid |
| 16 | 7.2 | Liquid |
| 17 | 6.5 | Liquid |
| 18 | 5.9 | Liquid |
| 19 | 5.3 | Liquid |
| 20 | 4.8 | Liquid |
| 21 | 4.3 | Liquid |
| 22 | 3.9 | Liquid |
| 23 | 3.5 | Liquid |
| 24 | 3.1 | Liquid |
| 25 | 2.8 | Liquid |
| 26 | 2.5 | Liquid |
| 27 | 2.2 | Liquid |
| 28 | 1.9 | Liquid |
| 29 | 1.7 | Liquid |
| 30 | 1.4 | Liquid |
| 31 | 1.2 | Liquid |
| 32 | 1 | Liquid |
| 33 | 0.8 | Liquid |
| 34 | 0.64 | Liquid |
| 35 | 0.5 | Liquid |
| 36 | 0.3 | Liquid |
| 37 | 0.15 | Liquid |
| 38 | 0 |
*Not all tablets are suitable to be halved. Check with your pharmacist or prescriber before doing this.
This information was produced by the Royal College of Psychiatrists’ Public Engagement Editorial Board (PEEB). It reflects the best available evidence at the time of writing.
Expert authors:
- Professor Wendy Burn, Past President, Royal College of Psychiatrists
- Dr Mark Abie Horowitz BA BSc MBBS MSc PhD, Clinical Research Fellow (NELFT), Honorary Clinical Research Fellow (UCL)
- George Roycroft, Head of Policy and Campaigns, Royal College of Psychiatrists
- Professor David Taylor MSc PhD FFRPS FRPharmS, Professor of Psychopharmacology (KCL)
We are grateful to the Royal College of General Practitioners (RCGP), the Royal Pharmaceutical Society (RPS) and the College of Mental Health Pharmacy (CMHP) for endorsing this work, and to all those who provided comments and supported its development.
Published: Mar 2024
© Royal College of Psychiatrists










