Dean's Grand Rounds

What are the Dean's Grand Rounds?
The Royal College of Psychiatrists Dean's Grand Rounds is a free webinar series that brings together clinicians, academics, and people with lived experience to explore challenges in clinical practice. The Dean's Grand Rounds aim to bridge the evidence-practice gap through an evidence-based, data-informed, and experience-driven approach.
Aims
The Dean's Grand Rounds aims to:
- Narrow the gap between education and practice;
- Empower clinicians to use data to understand and address challenges in their communities;
- Embed lived experience in clinical education and learning;
- Promote Quality Improvement (QI) approaches that are systematic, data-driven, and collaborative.
Together, these sessions help participants see how a problem-focused, data-informed approach can lead to meaningful change in mental health care.
Session Structure and Format
The Dean's Grand Rounds focuses on understanding a problem or opportunity for change through three lenses:
- Experience - insights from people with lived experience, carers and staff.
- Evidence - what research and best practice tells us.
- Data - contextual information that shows what's happening in practice.
By combining these perspectives, we explore how to bridge the evidence-practice gap and embed improvement.
Format: 90 minute webinar with Q&A and interactive discussion.
Audience: Open to all.

Collaboration and Values
The Dean's Grand Rounds is guided by Collaboration, Inclusion, and Learning.
Each session is developed jointly by Royal College of Psychiatrists Faculties, Special Interest Groups (SIGs), Regional and International Divisions and partner organisations (where possible).
We place a strong emphasis on:
- The voice of lived experience;
- Problem-focused inquiry;
- Data-driven understanding;
- Shared learning from both success and challenge.

Our Team
Contact us here.
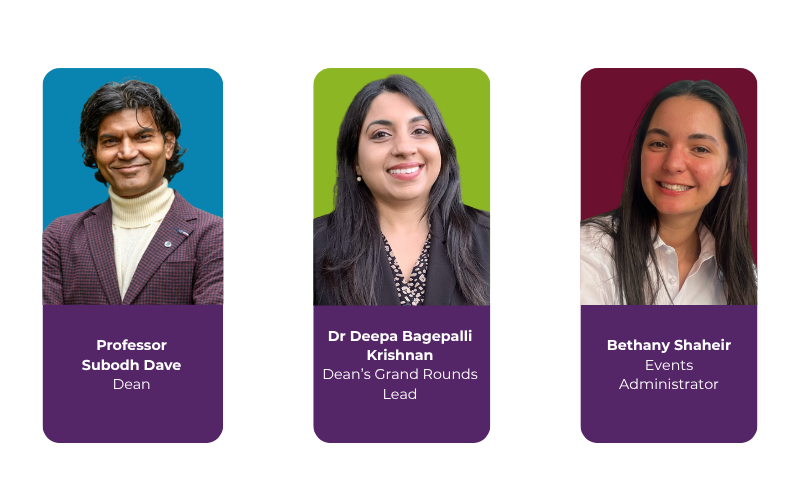
Professor Subodh Dave
Professor Subodh Dave was elected as Dean of the Royal College of Psychiatrists in 2021 and will hold the role until 2026. He has overall responsibility for setting standards for and facilitating the effective delivery of psychiatric education and training. He works as Consultant Liaison Psychiatrist in Derbyshire Healthcare Foundation Trust and is Professor of Psychiatry at the University of Bolton. He is passionate about ensuring that training, assessment structures and CPD (Continuing Professional Development) programmes lead to improvements in patient care and clinical outcomes.
Dr Deepa Bagepalli Krishnan
Dr Deepa Bagepalli Krishnan is a Consultant Perinatal Psychiatrist and Medical Quality Improvement (QI) Lead at Nottinghamshire Healthcare NHS Foundation Trust. She is also a part-time PhD student at the University of Nottingham. Deepa’s professional interests lie in quality improvement, leadership development, and medical education. Passionate about embedding QI principles into clinical practice, she has coached and led multiple award-winning projects that have delivered sustainable improvements at both regional and national levels.
Bethany Shaheir
Bethany Shaheir works in the Events Team at the Royal College of Psychiatrists. As the lead for the Grand Rounds within her team, she coordinates the planning and delivery of the series.
Submit an Expression of Interest
If you are interested in delivering a Dean's Grand Rounds webinar, please submit a proposal via this form.
The team will be in touch with you if we wish to take your proposal forward, and we can meet to discuss next steps.
If you have any questions, please email Bethany Shaheir.
Past Feedback
99% of attendees said that their 'Overall experience' at a Dean's Grand Round was 'Good' or 'Excellent', with 69% saying it was 'Excellent'.
Read more comments from attendees:
"Rich panel perspectives which I could have listened to for a long time. Given me some good ideas to support colleagues as well as patients. Very good."
"The testimony from a patient was [a] good idea to hear directly from service users."
"I loved how the cases made learning vivid, how the voices across disciplines enriched the dialogue, and how the interaction turned it into a true exchange of wisdom."
"Very thought provoking...Will look to learn from the webinar to change my practice."
Upcoming Sessions
Invisible in Plain Sight: Addressing the Mental Health Crisis Among Neurodiverse Youth and Rising Youth Violence - Thursday 26 February, 4.00pm - 5.30pm
This Grand Round will highlight where systems are failing, explore the structural, clinical, and social challenges that leave neurodiverse children and young adults unsupported, and bring together experts to identify the gaps and struggles. The session is not presenting a finished solution, but aims to foster discussion, share evidence and local data, and collaboratively consider upstream interventions to prevent crises before they occur.
One Pathway, Two Lives: integrating preconception and perinatal psychiatric care - Thursday 26 March, 4.00pm - 5.30pm
This Dean's Grand Round focusses on the role of preconception care in women with psychiatric disorders and models of perinatal psychiatric care in South Asian countries. Our discussions will be around current practice in the UK and South Asia for women with psychiatric disorders in the perinatal period as well as the challenges faced by psychiatrists and obstetricians related to preconception care. We will share lived experiences of women and the barriers faced by clinicians trained in the UK when they started specialised services in the Middle East and South Asia.
Past Sessions
2026
Special Committee on Human Rights in collaboration with the the RCPsych Working Group on Mental Health and Forced Migration explore the human rights implications of addressing the mental health needs of refugees and people seeking asylum.
In the UK, people seeking asylum and refugees make up around 13% of the immigrant population. This group experiences higher rates of psychological disorders which are exacerbated by unmet social needs. Mental health and social care services are however poorly equipped to provide appropriate care for this population. A national survey of UK-based psychiatrists showed that less than half the psychiatrists who responded considered themselves to possess adequate knowledge to treat patients from this group.
The Grand Rounds will aim to explore the human rights implications of this treatment gap, hear directly from advocates and service users, and offer actions to support psychiatrists in developing and maintaining the necessary skills to address the treatment gap.
2025
This symposium provides a practical overview of Gambling Disorder, including recent advances in research, policy, and practice.
Chair: Dr Lade Smith, speakers: Professor Sam Chamberlain, Professor Henrietta Bowden-Jones, Mr Steve Watts, Dr Konstantinos Ioannidis
This webinar describes the epidemiology of rising ketamine misuse and explain the consequences. It also outlines clinical responses and how to develop services. Talks cover: psychopharmacology, prevalence & adverse effects; Ketamine use in the community – case series including psychiatric vulnerabilities; Ketamine detoxification and severe dependence; developing a community ketamine service; and, developing an integrated service for ketamine users.
Speakers: Saul, Dr Emily Finch, Dr Irene Guerrini, Dr Faye Graver, Dr Stephen Kaar, Dr Tracey Myton.
The webinar, as part of the Dean's Grand Rounds, will explore the essential role of spirituality in mental health care. Recognising that spiritual beliefs and practices often shape patients' experiences of illness, suffering, and recovery, we will aim to equip clinicians with practical tools to take a compassionate, culturally sensitive spiritual history.
Smoking rates remain greatly elevated among people who use mental health services and is a [historically-neglected] source of profound health inequality. The NHS Plan correctly prioritises smoking cessation and this is a great opportunity to do something about this.
Researchers from the University of the York led the largest ever trial of a smoking cessation intervention in mental health services [the SCIMITAR trial]. In Bradford we have used evidence about ‘what works’ to drive culture change and to reduce health inequalities. Helping people who use mental health services to quit safely and effectively is central if we are to close the gap that exists in life expectancy.
Hear from research leaders and change agents working in the City of Culture 2025 [AKA Bradford]. Learn how we can move smoking cessation from ‘rhetoric to reality’.
Watch the webinar: Smoking and smoking cessation in mental health services
Exposure to and engagement in psychotherapeutic practice is central to person-centred compassionate good medical care and essential for psychiatric practice within the bio-psycho-social model and NICE guidance for the treatment of mental health problems and burn-out prevention.
This webinar discusses the results of a survey carried out to capture the views of our members about their experiences in everyday clinical practice and the opportunities available to employ and develop their psychotherapeutic knowledge and skills.
The desired outcome is reconnecting psychiatry to the bio-psycho-social model. In the long term, the hope is to deepen training, research and practice of psychotherapeutic and relational models within psychiatry. This is essential for future-proofing psychiatry, improving patient outcomes and retaining psychiatry by enhancing the meaningful aspects of their roles.
Social factors, stigma and cultural differences in how mental health is perceived are known to affect access to healthcare. Regional and remote areas bring unique challenges.
Two services in the UK (ROSHNI) and Australia (E-PIMH) will present how they have adapted their models of care to improve access to perinatal infant mental health services considering the unique needs of their communities.
ROSHNI is a national scale research study, designed to address the rise of British South Asian (BSA) women who experience post-natal depression.
E-PIMH is a Telepsychiatry service run by Queensland Centre for Perinatal & Infant Mental Health, providing specialist perinatal and infant mental health psychiatry across regional and remote areas with limited service access.
2024
In South Africa, the prevalence of perinatal depression is as high as 32%, meaning that almost 1 in 3 pregnant women have some form of perinatal mental illness. Despite this alarming statistic, there are still limited perinatal mental health services available and there is poor screening during the antenatal period for common perinatal mental health problems.
Pregnant women with mental illness go on to have poor maternal, obstetric, and neonatal outcomes; however, this experience is not unique to South Africa. Globally, racially and ethnically minoritized women disproportionately experience poor perinatal mental health care as a result of various factors, including stigma and psychosocial determinants of mental illness. Overall, this results in increased morbidity and mortality for the mother and baby, which is poorly documented and researched.
Public health awareness, education, and screening is often skewed towards ensuring physical safety outcomes, without consideration of integrating mental health supports in perinatal services and well-baby spaces. This webinar focuses on how to address the challenges of providing integrated perinatal and infant mental health services in resource-constrained settings by highlighting clinical, educational, and research opportunities in South Africa.
Whilst pregnancy and the first year of the baby’s life can bring joy, it can also be a period when some mothers experience mental health related problems for the first time.
Neurodivergent women in particular may face challenges which they have not dealt with before getting pregnant and looking after a baby.
With the increased awareness and understanding of neurodiversity in the population, more needs to be done to understand the needs of neurodivergent women in this critical period of their life and the lives of their families.
This webinar will consider what we know about ADHD and Autism in the perinatal period as well as identify areas for further research.
Mental health services for the elderly are not readily available in many developing countries, and there is a shortage of geriatric psychiatrists. This is a growing concern as the number of ageing people in these countries is increasing, and non-communicable risk factors associated with dementia, such as diabetes, uncontrolled hypertension, and obesity, are on the rise. Although general psychiatrists, neurologists and family physicians are available, their numbers are small, and they cannot provide comprehensive care for patients with dementia. In this regard, primary care services are better placed to deliver dementia services in low- and middle-income countries. The primary care workforce, including general practitioners and nurses, can be trained to offer holistic care for dementia patients and refer them to psychiatrists. This task-shifting is necessary to triage, treat, and address co-morbid medical and psychiatric disorders among patients with dementia. Moreover, it can provide links to community public health services to reduce risk factors, raise awareness and help communities to take care of patients with dementia.
In collaboration with the World Network of Psychiatric Trainees.
How should psychiatrists successfully advocate to impact policy and instigate change?
Staff working in healthcare settings experience significant work-related mental health distress. An interplay of a number of personal, occupational and socio-environmental factors results in high rates of burnout and mental health problems amongst physicians.
This session of Dean’s Grand Rounds focused on exploring and understanding this problem through physician experience, case studies and local data. The session also focused on some unique challenges in low and middle income countries and barriers to seeking mental health support amongst physicians.
We heard about an innovative approach developed in the National Institute of Mental Health and Neuro Sciences (NIMHANS), India to enhance physician wellbeing.

