Community mental health transformation: opportunities and challenges
05 January, 2022
Dr Helen Crimlisk and Rosanna Flury reflect on how services are changing, and how we can make the most of this new opportunity to improve care for patients.
Integrated care to address gaps in provision


It is an exciting time for Community Mental Health services.
The NHS Long Term Plan addresses gaps in provision of care which mean many patients with severe mental illness don’t get the care they need or fall through the cracks. Psychiatrists are often also frustrated by the rigid way in which services are commissioned and whilst many services provide good elements of care, they often use governance and service specifications which are not integrated.
There is a need to pay more attention to people’s experience in navigating community mental health services as well as specialist services for eating disorders, substance misuse and rehabilitation, and ensure that more patients get the right care without having to navigate multiple service boundaries with reassessments at every juncture.
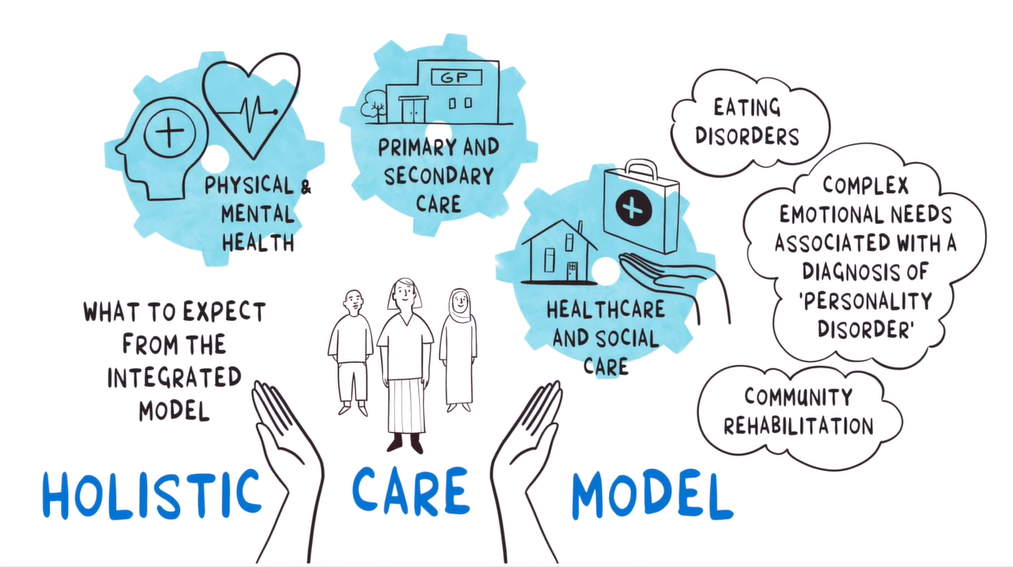
Transformation means holistic care and co-production

The community mental health transformation Programme has been co-designed with service users and carers nationally in association with the National Collaborating Centre for Mental Health. During the pandemic, 12 trusts in England started work on their transformation and the learning from these trusts has informed the rollout of the programme across England.
Because of the focus on co-production and the need for locally relevant services, each area will be co-designing their transformation with their local partners. This means there is no “blueprint” to follow and there is a need for systems leadership across the partners from secondary care, primary care, the voluntary, community and social enterprise (VCSE) sector and social care.
Other changes include the discontinuation of the Care Programme Approach and a focus on population-based early interventions and prevention, mapped on to Primary Care Networks which serve between 30 and 50 thousand people.
Equality of access and personalised care


The transformation comes with significant increased funding (£2.9 billion over 3 years) and this will be used to employ and train new staff working across the system with up to 50% of the funding going to the VCSE sector.
Provision will emphasise equality of access and culturally appropriate care, particularly for people from communities traditionally not well served. There will be roles for people to be supported to access a broad range of support and to provide a range of evidence-based therapies and interventions.
Learning from early adopters and the College Engagement Network
The national roll out started in 2021 and was informed by the learning of 12 early adopters. They have undertaken the work in very different ways but there is common learning which will be taken forward. The College Engagement Network (CEN) has been working with psychiatrists from these trusts to learn about the successes and challenges and to provide support in leading this transformation.
It has been very useful to have faculty and regional support in the CEN as well as the input of the College Presidential Lead for Primary Care and Community Assets, Professor Linda Gask and the Specialist Lead for Coaching and Mentoring, Dr Jan Birtle who has been supporting the group working on systematic leadership skills and developing action learning sets.

The challenge for psychiatrists
The ambition of the transformation is enormous. It aims at a blurring of boundaries between primary and secondary care, the integration of traditionally separately governed stakeholders, significant alliance building and increase in the involvement of VCSE with associated issues around power, culture and risk sharing and the employment and training of a number of new staff in new roles.
Transformation only works across systems and this means that clinicians in all mental health services and the psychiatrists within them will need to work differently too. There will be a greater need for relationship building, cross sector working, formal and informal supervision.
As psychiatrists, many of you will have a good appreciation of the power of co-production and recognise the value of people with lived experience. Nevertheless, this challenges us all to take this to another level, working with patients, carers and the VCSE in a way which really transfers power and resources to enable transformational change and shifts in power. Services will have to think more about digital systems and data collection to demonstrate the impact on outcomes.
A group within the College is currently looking at the implications for consultant psychiatry job plans, and consideration will also need to be given to ensure that all psychiatrists (trainees, SAS doctors and consultants) are supported to develop the necessary skills to work differently, which should link in well with the enhanced focus on leadership development and co-production being emphasised within the College.
To get an idea of the ambition, take a look at this five-minute film.

Authored by Dr Helen Crimlisk and Rosanna Flury.

